9 Practice-Based Research and Learning Networks (PBRLNs) across 7 provinces.
Background
Background
Healthcare costs consume an alarming proportion of the gross domestic product (GDP) in Canada, increasing from 7% to 11% over a 40-year period. Half to two-thirds of healthcare costs in Canada are incurred by 5% of the population. Some of those patients are elders living with multiple chronic conditions; they may have unmet care needs. These patients may take many medications, some of which do not benefit them.Ananalysis of the University of Toronto Practice-Based Research Network’s (UTOPIAN’s) electronic medical record (EMR) data revealed that each family physician looks after, on average, 24 elderly patients who were prescribed ten or more different medications in the past year. Polypharmacy can be associated with elevated risks of poor health, reduced quality of life, high system costs as well as frustration for physicians.
Our proposal
We propose SPIDER: a Structured Process Informed by Data, Evidence and Research as a method to improve health care for these complex patients. The overarching goal of the study is to assess whether SPIDER will improve care by empowering patients and physicians so that they can have more meaningful discussions about medications prescribed and taken. Taking a significant number of medications has been called “polypharmacy”—and some medications could and should be stopped. Decreasing polypharmacy could lead to improvements in patients' overall care and health and, as a result, a greater workplace satisfaction for physicians and others involved in the care of complex patients.
Our targeted medications
While a number of medications are problematic, the following medications have been identified by Choosing Wisely Canada and the Canadian Deprescribing Network as targets for wiser use in elders: proton pump inhibitors (PPIs) that reduce stomach acid production, sedative hypnotics such as benzodiazepines, antipsychotics for agitation and medications associated with higher risk of low blood sugar such as long-acting sulfonylureas.
Improving patient care by combining QI and research methods
An important area of practice transformation is systematic improvement of the quality of patient care. Quality improvement (QI) is an applied science that focuses on measurement and rapid-cycle tests of change in each local context while emphasizing sustainability and spread of effective change within and across healthcare systems. A complementary approach is that used in many research projects: follow rigorous steps to systematically collect evidence about the effectiveness of interventions implemented in the same way across multiple settings. SPIDER leverages existing relationships between QI experts and researchers and uses both approaches. SPIDER is jointly supported by Practice Based Research Networks (PBRNs) and QI programs and backed by research ready EMR data to improve care in primary care.
The number of medications prescribed to a patient is the single most reliable index of high care costs over 3 years
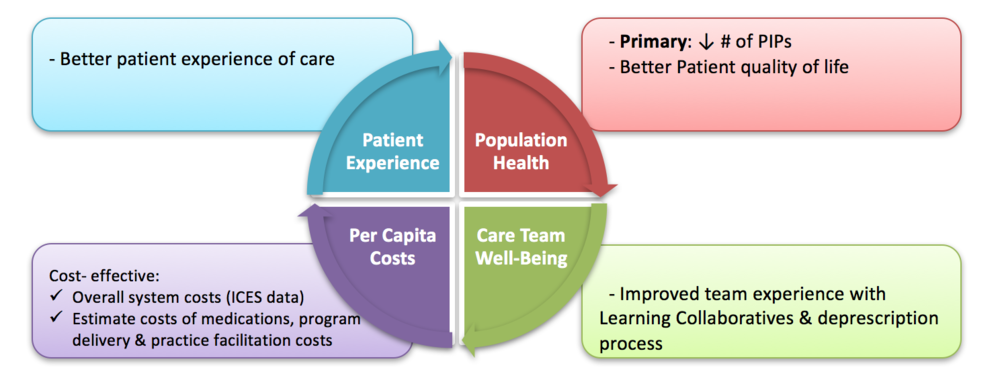
SPIDER’s quadruple aim and outcome measures